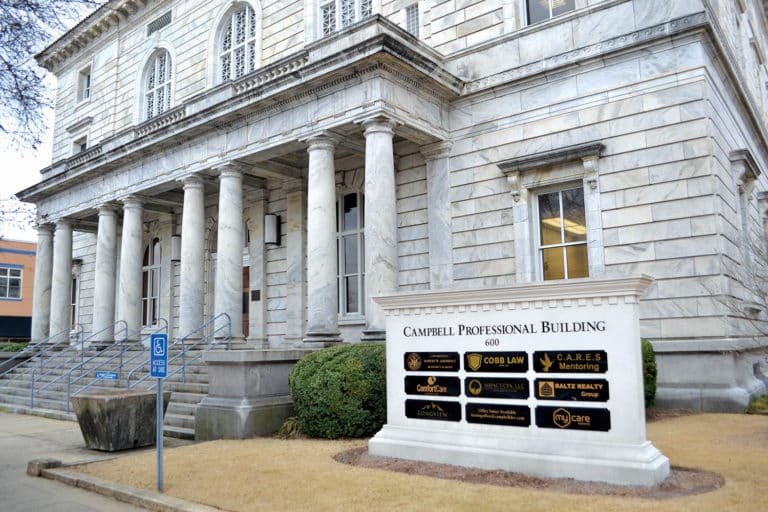
Photo: The Federal Building in downtown Gadsden holds Comfort Care Hospice, among other businesses. (Emma Kirkemier/Messenger)
01-12-2023
By Emma Kirkemier, News Editor
Countless families in our community have been faced with the hard decision of enrolling a loved one in hospice care. Over a dozen hospice providers operate in Gadsden alone. According to local practitioners, however, most do not fully understand hospice care.
Erin Davis of Comfort Care Hospice explained that few patients are aware of the manifold benefits offered in hospice, and still fewer are open to talking about it. Davis’ job as account executive is to serve as a liaison between the patients, the public and the provider.
“Hospice is not the end,” Davis said. “You have to be at a certain progression of your disease, but it doesn’t have to be actively dying.”
According to Davis, who is also a registered respiratory therapist, hospice care is not just for those at death’s door, but for anyone diagnosed with a “life-limiting illness.”
“It’s quality versus quantity,” she said. “We want you to live your life with the life that you have left to live. We want you to have everything (you need).”
Davis claimed that the hesitation or outright denial many caregivers display around the topic of hospice is actually part of its prevalent stigma.
“A lot of times people associate hospice with just immediate death because they wait until the end to put the patient, their family member, on hospice,” she said. “[When a patient accepts hospice earlier in the progression of their illness,] you can get to know your nurses and get to know your aides. Vice versa, they get to know the family. My nurses are wonderful, and most hospice nurses are. They just love people, and they just want to take care of them.”
Similarly, many families are unfamiliar with the full scope of the care offered.
The Alabama Department of Public Health defines hospice as “a coordinated program of home, outpatient and inpatient care and services … in order to meet the physical, psychological, social, spiritual and other special needs that are experienced during the final stages of illness, dying and bereavement.”
The American Cancer Society writes this about hospice care:
“Hospice care provides compassionate care for people in the last phases of incurable disease so that they may live as fully and comfortably as possible. The hospice philosophy accepts death as the final stage of life: it affirms life, but does not try to hasten or postpone death. Hospice care treats the person and symptoms of the disease, rather than treating the disease itself. A team of professionals work together to manage symptoms so that a person’s last days may be spent with dignity and quality, surrounded by their loved ones. Hospice care is also family-centered – it includes the patient and the family in making decisions.”
Hospice care is not only for the patient, but for their caregivers. Many hospice services offer respite care, which provides a break for caretakers by assuming full care of the patient for a limited time. Some also provide counseling for the family, even after a patient’s death.
Davis said Comfort Care employs a social worker and a chaplain who work closely with families.
“It’s a benefit of Medicare,” Davis explained. “Everybody who has Medicare is entitled to hospice. It will pay for your medication that’s related to your diagnosis. It will pay for all your home equipment. Nurses will come into your home two to five times a week.”
Davis said that many patients are unaware of the benefits to which they are entitled through their insurance, as most insurance providers cover hospice care. Hospice staff will often set up the necessary home equipment as well.
According to Davis, these practical and financial benefits are a substantial part of enabling patients to get the best possible care for maintaining quality of life.
“Especially with our older people who are on budgets where they don’t have all this extra income, we’re going to pay for a majority of your meds,” she said. “There will be certain ones that we can’t pay for, but anything related to your diagnosis (we can).”
Davis explained that when a patient begins receiving hospice care, aggressive treatment of their illness has ceased. However, healthcare workers will continue to treat their symptoms, as well as any other ailments that may arise. Hospice providers can pay for necessary auxiliary medications including pain medicine, inhalers, antidepressants and antianxiety medications.
“We absolutely will never put a patient on hospice if they do not need hospice,” Davis said. “But what’s worse, even more so, is not putting a patient on hospice when they’re hospice-appropriate, because that is robbing them of a benefit that they are entitled to and a service that’s beautiful.”
Davis praised the Comfort Care nurses for their exemplary care, especially their involvement with long-term patients.
“Your family member or loved one who is slowly dying is now getting the chance, the longer you have, to have that personal relationship with someone taking care of them who they know is going to be with them when they die,” she said. “You don’t want a stranger to do that. You want someone who you love. Our nurses have been with some of our patients for years.
They’ll go to their funerals. They’ll be with (their families). They’re very involved with their families; they love them.”
Sometimes hospice patients improve to the point that they can resume treatment, or at least revisit their plan of care. In these cases, Comfort Care will move the patient to a home healthcare program.
“Our home health and hospice work hand-in-hand,” Davis said. “If a patient is doing really well in hospice and they’re improving, we’ll flip them to home health. It’s not an end. And then in home health if they see that they’re not improving like they should, we’ll start having the hospice conversation.”
That conversation, she said, is often eye-opening for both patients and caregivers. Davis has talked with multiple patients who outright refused hospice care, only for them to change their minds upon learning more.
According to Davis, hospice is about personalized care above all else; whatever treatment a hospice patient receives will be “the best thing for them.”
“It’s the freedom that hospice gives patients,” Davis said. “It gives you more autonomy over your own existence. We allow you to live your life, and we want to make you comfortable. We are not trying to hasten it. We’re not slowing it down; we’re not speeding it up. Whatever time left the Lord intends for you, we want to make it the best it is.”